Perimenopause (or nearing menopause) is a natural transition that affects each person differently. Menopause is marked by the final menstrual period; one is considered in menopause after twelve months with no periods.
Perimenopause & Menopause
- 20

Growing Older Menstruation through Menopause
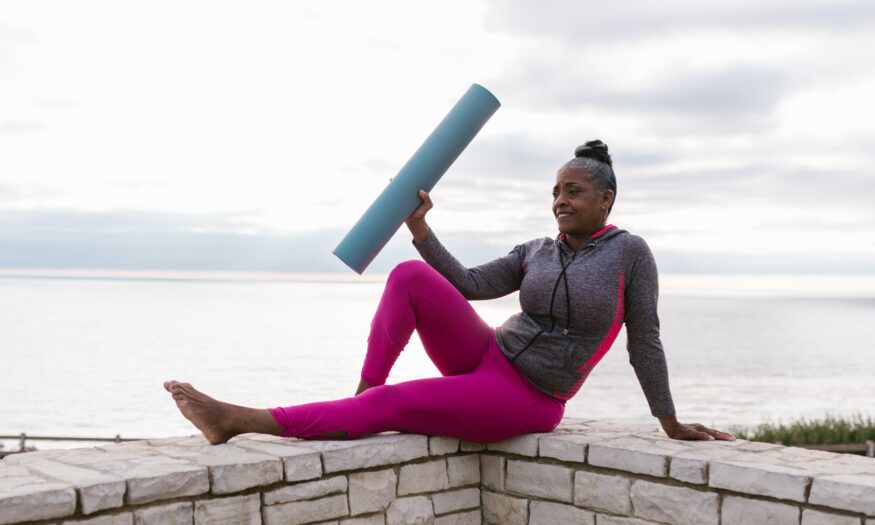
“Decolonizing The Crone” and Reclaiming The Freedom of Aging

Menstruation through Menopause
Living in Uncertain Times: Experiences of Menopause and Reproductive Aging
Menstruation through Menopause
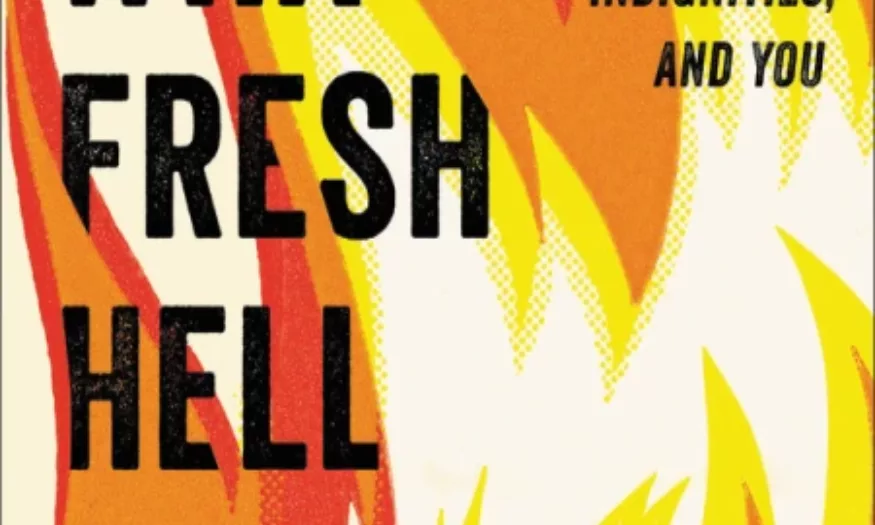
What Fresh Hell Is This? Perimenopause, Menopause, Other Indignities, and You

Menstruation through Menopause
Who Knows When My Period Will Arrive Next?: A Conversation about Menopause